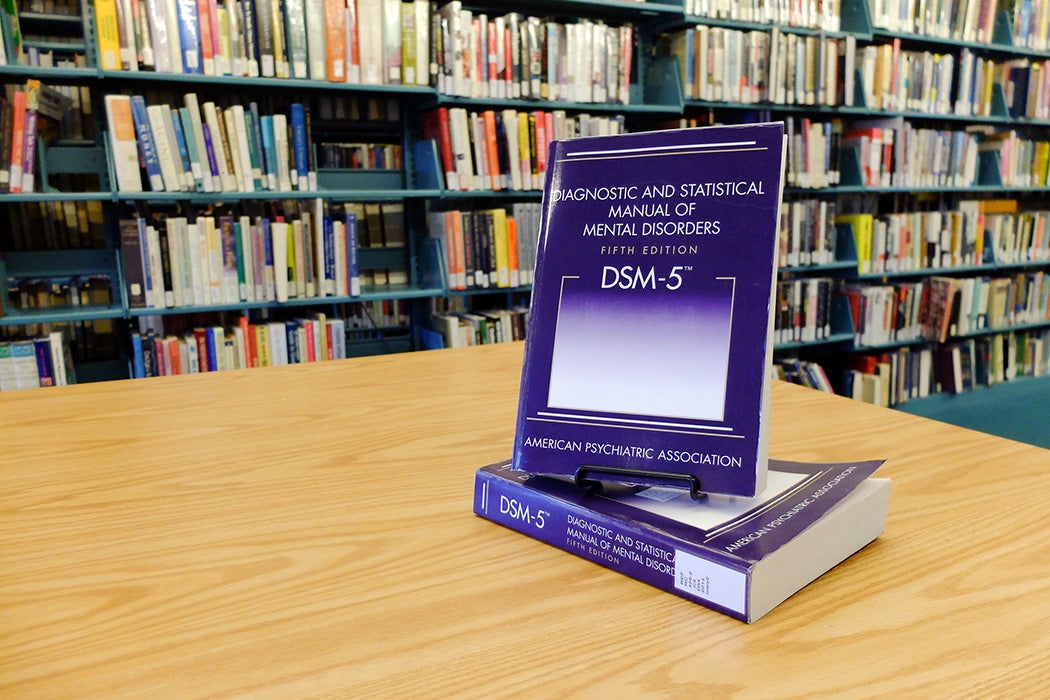
In recent years, corners of the internet concerned with mental health have been debating whether it’s appropriate for people to “self-diagnose” conditions from anxiety to autism based on things they learn on social media. But even professional diagnoses are complicated things, with criteria that change over time and are subject to debate among experts. In 2014, a package of articles published by the Journal of Medical Ethics explored some of these issues in relation to the then-new Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
In his contribution, Martyn D. Pickersgill, a sociologist of science and medicine, pointed out that the DSM-5, published by the American Psychiatric Association (APA), received criticism from people inside and outside the mental health professions for its supposed medicalization of normality. For example, it eliminated a recommendation found in previous editions of the DSM that clinicians shouldn’t diagnose major depressive disorders in anyone who had recently experienced the death of a loved one. Many bristled at the idea that the “everyday experience” of grief could be identified as a mental disorder.
A related criticism Pickersgill points to is that psychiatric diagnoses, often defined based on a cluster of symptoms, are less definitive than determinations of many physical illnesses based on objective biomarkers. In practice, he writes, many mental health providers consider a DSM diagnosis a “convenient fiction” that helps them communicate with patients about their needs, rather than a definitive description of an objectively identifiable condition.
This points to the question of the purpose of a diagnosis, which is taken up by psychiatric researcher George Szmukler. He writes that there are a number of answers. Most obviously, it can help a care provider determine the most appropriate treatment for a patient or structure the work of researchers.
In other cases, Szmukler writes, a diagnosis’s real purpose doesn’t involve the person’s “status” in a particular diagnostic category but their “function”—the things of which they’re capable. One example is involuntary medical treatment, which could be justified based on a person’s lack of decision-making capacity, regardless of whether the person has dementia, stroke, or schizophrenia. Another is entitlement to public benefits like housing or cash aid, where the relevant question is what type of assistance a person needs.
Weekly Newsletter
In her contribution, Felicity Callard, a medical humanities scholar, considers her own experiences receiving mental health diagnoses from various providers. She notes that some critics view certain mental health issues as an issue not of illness but of social stigmatization, as in the case of homosexuality previously being identified as a disorder.
However, she suggests that it’s worth occupying a position of ambivalence about the “reality” of any given diagnosis. Putting a name to a problem may not define it permanently or objectively, but it can serve purposes from getting a desired treatment covered by insurance to helping a person structure their understanding of themself and find communities of people in similar situations.