People with mental illness frequently face abuse and neglect—including from the health care systems that are supposed to be helping them. But, as anthropologist Athena Helen McLean writes, for decades they’ve been fighting back. Their organizing strategies have ranged from radical opposition to the medical establishment to efforts to exert consumer power within it.
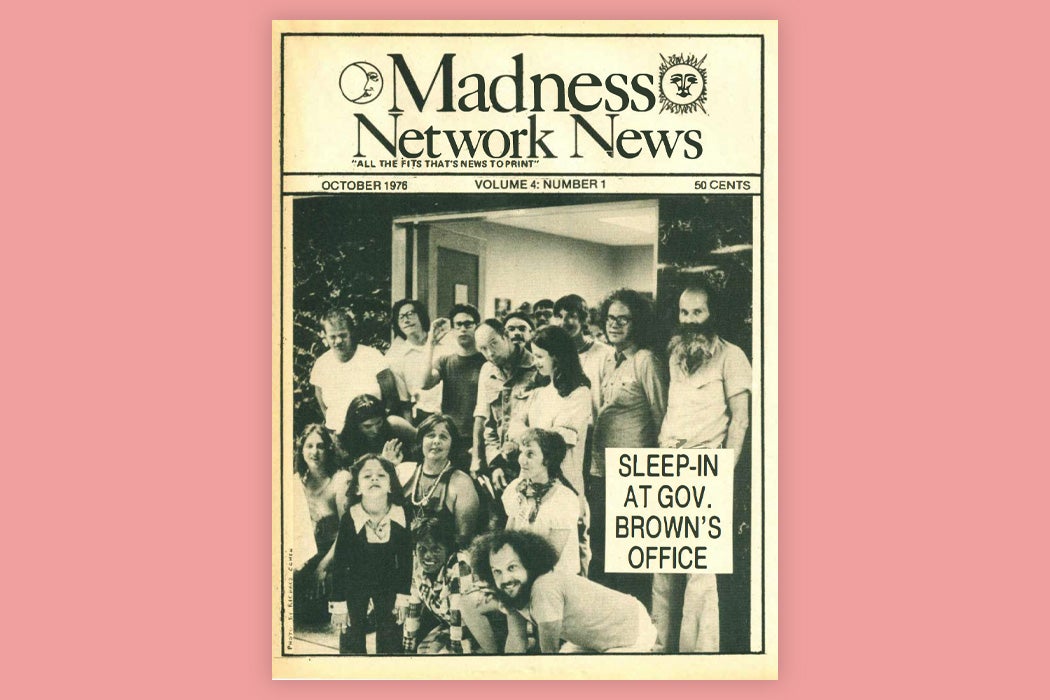
In the 1970s, McLean writes, former patients mobilized through the Psychiatric Inmates Liberation Movement, which modeled itself on other civil and human rights movements of the time. Many of the organizers of this work were people from middle- or upper-class families who had been forced into hospitals as young adults. Much like in the consciousness raising groups of the women’s liberation movement, when ex-patients gathered and shared their stories, they often found their feelings of injustice validated. With a new sense of empowerment and self-determination, they found their conditions improving.
These activists tended to oppose not just involuntary commitment and forced treatment but the medical model of illness overall. Instead, they generally saw the roots of their problems in societal oppression. Here, gay liberation offered a model of fighting the medical stigmatization of human diversity.
In the late 1970s, the National Institute of Mental Health (NIMH) created the Community Support Program (CSP) in an effort to rebuild services for people with mental illness as they were released from long-term institutions during the era’s mass deinstitutionalization. The CSP focused largely on winning broad support for community treatment options with the help of the families of mentally ill people, but it did also work with members of the ex-patient movement. Through this engagement, people with mental illnesses formed connections with officials in the mental health system, influencing institutions and promoting new, consumer-run alternative mental health programs. Meanwhile, increasing numbers of mentally ill people began viewing themselves as empowered consumers, learning about treatment options and their own legal rights and using this knowledge to influence institutions.
“The new consumer did not experience the same extremes of helplessness and oppression as did the founders of the ex-patient movement,” McLean writes. “Many in fact valued the provide-consumer relation and wanted to support it, not challenge it, in their work as consumer advocates.”
This increasing integration with mental health systems allowed mentally ill advocates and activists to reach more people, including mental health consumers, policymakers, and the broader public. But, at the same time, many patient-run alternative organizations became dependent on government funding and subject to political forces, which pushed them to focus on providing treatment rather than taking on broader social goals.
Weekly Newsletter
“The ‘warm, human contact,’ consciousness-raising, advocacy, and anti-authoritarian self-help willingly shared in a local group can be undercut by funding intent on extending indigenous ‘expertise’ to a wider net of ‘consumers,’” McLean notes.
Today, mental health activists and advocates continue to pursue a variety of strategies, from mutual aid to fighting from within the system, to win better care and greater dignity.
Support JSTOR Daily! Join our new membership program on Patreon today.