It was a dire situation. A young boy with a rare condition was losing skin. Soon he had lost the majority of skin on his body. Wracked by sepsis and losing weight, the boy was near death. But a novel treatment saved his life—an artificial skin produced from the boy himself.
Healing severely damaged skin has long been difficult. While the genetic condition that almost took the boy’s life is uncommon, injuries and illnesses such as burns, severe abrasions, and diabetic ulcers are very common. Skin forms a protective barrier; when that barrier is damaged infection becomes a major risk. Burns in particular can cover large areas and are very difficult to keep clean.
When possible, pieces of healthy skin from elsewhere on the body are grafted over the damaged area. Before the possibility of growing actual replacement skin, the priority was a temporary covering that could help a patient stay alive until they can heal a bit. There are many possibilities, many of which have been successfully used as a temporary barrier. Some of these are not pleasant in concept. Skin from human cadavers has been used for years, as have frog and pig skin.
Given the variation in types of skin wounds, several products have been bioengineered, tailored to different wound types. These are designed for either use as a temporary cover in healing or as a permanent replacement for missing skin. Some of these involve modifying cadaver skin to improve its function. Several involve different configurations of pig or cow collagen mixed with human cells or proteins. At least one product is like something out of science fiction: pig collagen in a silicone matrix. Proteins called epidermal growth factors that help encourage growth and repair of tissue are also used.
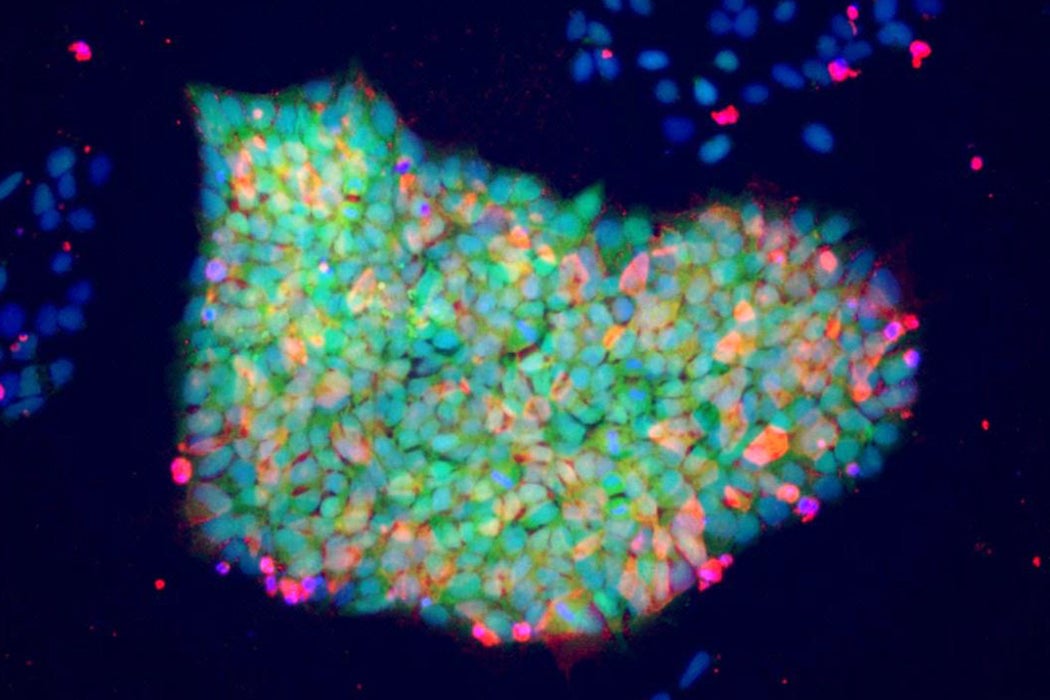
Any treatment that is not derived from the patient’s own tissue poses risks of disease transmission or incompatibility. Non-human products pose risks of dangerous allergic reactions. This new treatment is the first to be derived from pluripotent stem cells, cells that are capable of turning into multiple different tissues in the body. The skin was grown in huge sheets, coaxed into being from these malleable cells.
But the boy’s treatment, and all bioengineered solutions, do have a drawback. They are extremely expensive. If these treatments find wider success, the cost may come down. Until then, these lifesaving strategies might be out of reach for many people.