The United States has a long love affair with psychotropic drugs: from Valium to Prozac to Xanax, it seems that prescription brands come in and out of fashion almost like clothing lines.
Many patients’ lives are immensely improved (or in some cases, saved) by one tablet, two times a day. At the same time, psychiatrists and the medical community have, for the last few years, been pushing back against our increasing propensity to treat the ordinary human condition.
The line between distress and disease is blurry, but it is nonetheless a vital distinction. In the International Journal of Feminist Approaches to Bioethics, scholar Ami Harbin suggests that modern medicine is in danger of pathologizing what are painful, but normal, human experiences—what she calls “disorientations”—and doing patients a disservice in the process.
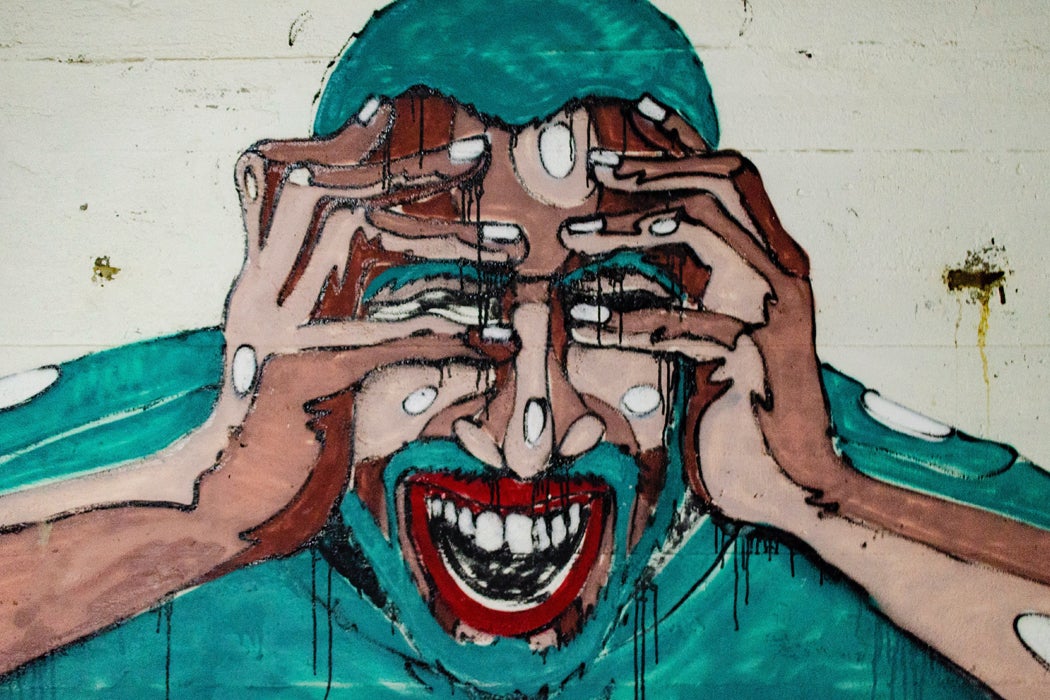
Harbin describes disorientation as feeling “uneasy, uncomfortable, and not at home in body, affect, and thought.” She writes that an individual can be thrown into disorientation through sudden change, like bereavement or illness or the end of a relationship or a job. Or, more insidiously, they “may instead grow out of a more subtle and persistent tension or ill fit between an individual and characteristics of the social world, like the disorientations that may result from being non-white in a racist world, or being a queer teen in a heteronormative high school.”
She notes:
Positioning such experiences as primarily objects of medical or psychiatric discussion, rather than as expected parts of non-pathological emotional life, can mean that the complexity of such experiences gets lost, and…can, in some cases, make such experiences more likely to harm individuals than they otherwise would be.
One such example is the clinical imposition of a time limit on “normal” grief: after a matter of weeks following the death of a loved one, sleep disturbances, changes in appetite, loss of energy and persistent feelings of sadness become clinical symptoms of depression—not features of the healthy (albeit excruciating) path to healing.
Get Our Newsletter
Harbin clarifies that, “Clinicians will be given advice about how to distinguish normal grief from depression in these instances, but the shift in diagnostic criteria is worrisome to its critics for the way it may err on the side of overdiagnosis of depression and under-awareness of the nonpathological difficulties of grief.” She adds that medical professionals ought to acknowledge that stressful situations like loss, illness, new responsibilities, and changing relationships are likely to be greeted with “disorientations,” or serious emotional struggle.
Harbin is careful not to lay the blame on solely on the medical industry or physicians themselves. Pathology is a social construct as well as a medical one. She writes, “medicalization is not the work of medical professionals alone: it is the product of the participation of many individuals (family, friends), institutions (schools, workplaces), and systems (justice systems, social-security systems).”
In other words, well-meaning though we may be, we may be quick to label someone as mentally ill because they think or act differently; someone as clinically depressed when they’re processing a traumatic event, someone as “stuck” if they grieve for longer than we want them to.
This isn’t to say medical intervention isn’t sometimes necessary: ADHD medication and anti-depressants have an important place and serve a crucial function ifor many. But, according to Harbin, each and every one of us—not just physicians—have a responsibility to ensure we’re not rushing to fix loved ones when they’re in no need of repair.