In summer 2019, months before the novel coronavirus put the planet into lockdown, people in Massachusetts and Connecticut began to die from a strange illness. Seemingly out of the blue, they would develop severe headaches, high fevers, and muscular twitching. They would also become drowsy, irritable, and complain about stiff necks. As the disease developed, they would have convulsions and fall into a coma. One Connecticut patient died. Within a few weeks, two more deaths followed. In Massachusetts, a woman died from the same illness. There were cases in other states too.
Doctors diagnosed these patients with Eastern Equine Encephalitis or EEE—a rare but often-fatal brain infection typically characterized by high fevers, headaches, and neurological issues. Spread by mosquitoes and caused by a virus that attacks the brain and the nervous system, the infection kills about 30 percent of patients; those who survive it often battle neurological problems afterwards. This summer, people weary of lockdowns are flocking to nature seeking respite among the trees, lakes, and creeks. But is it safe to wander outdoors?
EEE may sound like yet another new scourge that caught humans by surprise, but unlike the novel coronavirus, it isn’t novel at all. The earliest recording of the conditions was likely observed in horses in 1831—hence the name “equine.” But it wasn’t until a century later that the disease became a recognized problem and got an official name. EEE proved to be very fatal—in some locales up to 90 percent of infected animals died. Scientists also identified a Western equine encephalitis and St. Louis encephalitis—slightly different strains but with similar morbid symptoms and outcomes. During the 1930s, the disease killed thousands of horses in North America. The Canadian province of Saskatchewan alone lost somewhere between 13,000 and 15,000 animals. And human cases began to appear too.
In August of 1938, Massachusetts was struck by the epidemic of equine encephalitis—and then children started falling ill with somewhat similar symptoms. They developed headaches, high fevers, convulsions and often would be in a coma by the time they arrived at a hospital. The disease turned out to be lethal–one child died on August 12 and another one from the same city on August 30. More cases followed and while they seemed to be happening miles away from each other, they all were occurring within the same geographical area as the equine disease. Rumors began to circulate that the equine scourge had jumped to humans. Rumors proved correct. Humans were falling ill and dying from equine encephalitis too, confirmed a paper published in American Public Health Association Press. But while some link between horses and humans had been established, the exact mode of transmission was still unclear.
John S. Fulton who studied the epidemiology of the disease in Saskatchewan, observed that the majority of people who fell ill with equine encephalitis were farmers, many of whom had been in close contact with sick horses. But, he also noted that some patients weren’t anywhere near the afflicted farms. They lived in towns and villages and had not been in contact with diseased animals. In many cases they hadn’t been in any contact with animals at all.
A 1933 hypothesis postulated that pigeons were the natural carriers of the virus. In 1938, scientists proved this to be correct, after the virus was found in a wild pigeon in Massachusetts. That same year, scientists also found it in wild pheasants in Connecticut. It turned out that most bird species, with a few exceptions, tolerated the virus well, and either recovered quickly or didn’t get ill at all. That made them natural reservoirs for the virus.
Figuring out exactly how the virus spread from birds to horses to humans took a bit longer. By the 1930s, scientists knew that insects could spread disease by bites. In 1897, French military surgeon Alphonse Laveran and British bacteriologist Ronald Ross elucidated how several species of mosquitoes harbored and passed on the malaria parasite Plasmodium. So insects were natural suspects, but it wasn’t clear which ones. Fulton’s paper linked the possible cause to biting flies or mosquitoes, but ultimately didn’t draw a conclusion. “It would appear that there is no correlation between the incidence of the disease, the presence or absence of mosquitoes, amount of rainfall, or topography of the country,” wrote Fulton. “In fact, we must admit total ignorance of how the disease is spread from infected to healthy animals, or how the virus is carried over from year to year.”
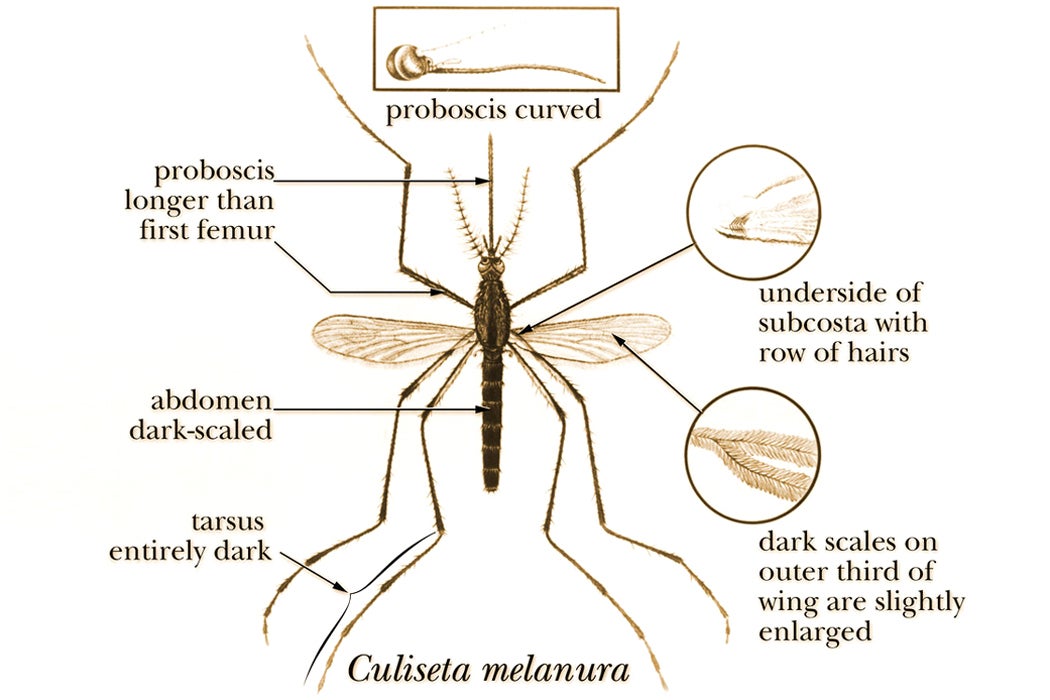
By 1959, studies named the bog mosquito Culiseta melanura as the primary encephalitis vector. An ornithophilic mosquito—which means that it feeds primarily on birds—C. melanura rarely bites people, which is why EEE is so rare. As part of its lifecycle, the EEE virus circulates between the C. melanura mosquito and birds, rarely spilling onto other animals. C. melanura is very particular about its breeding places—it prefers secluded shady areas and the cool, acidic water of freshwater swamps. This kept the EEE virus contained in those places. But heavy rains can somehow offset that balance, leading to an increase in the mosquito population. Other mosquito species can pick up the virus from the birds—and spread it around, leading to outbreaks in horses or humans. Both 1938 and 1955 outbreaks in Massachusetts occurred after unusually massive rainfalls. But when Massachusetts experienced an extreme summer drought in 1957, there were no reported cases of EEE in humans or horses.
That makes encephalitis an epizootic disease, which means that it periodically arises in animal populations—and eventually disappears. That’s exactly what equine encephalitis did historically—it spiked and vanished several times over the years. While the 1930s outbreaks petered out, it peaked up again in 1965, when Centers for Disease Control and Prevention registered cases in several states. Two people have died in Georgia. In August of 1989, 11 states reported to the CDC 65 equine incidents of eastern equine encephalitis, and one human case—an 11-year-old boy in Mississippi who died.
Notably, horses and humans weren’t the only victims of the equine encephalitis—some birds weren’t immune to it either. In 1991, when heavy rains in southern Louisiana spawned a large population of mosquitoes causing an EEE outbreak in horses, a flock of bred emus also succumbed to the disease. Unlike most wild birds that develop antibodies to the virus, the emus didn’t do well. They became depressed, had bloody diarrhea, and over 80 percent of them died. A 31-year old male seal from a Massachusetts zoo that stopped eating and suddenly developed seizures. Notably, other four seals he lived with did not seem to be affected.
Weekly Newsletter
In 2005, cases of human eastern equine encephalitis peaked again. From August to September of 2005, seven people were diagnosed with it in New Hampshire and four in Massachusetts—and four of them died. All the patients lived in wooded areas and spent some time around the cranberry bogs, wetlands, or swampy areas where mosquitoes were in abundance. And then there was a relative lull in cases—until 2019, when Centers for Disease Control registered 34 cases of EEE in seven different states. The New England Journal of Medicine noted that it was the largest EEE outbreak since the 1930s.
That means that we may be in for another epizootic spike this year. Of course, EEE poses less danger to humans than the coronavirus. It is much deadlier than COVID-19, but the EEE virus itself is much easier to avoid. Luckily, it can only be transported between animals through mosquito bites, and mosquitoes can be kept away with insect repellant, pesticides, clothes that cover one’s skin and other means.