To a handful of medical historians and doctors, the name Ibn al-Nafis gently tugs at the heartstrings, but for most, it is undoubtedly unfamiliar. Ibn al-Nafis did what so many medical thinkers and doctors could not: He correctly explained how the heart pumps blood, and he did so centuries before the advent of modern medicine. Although the discovery of the heart’s true anatomy is commonly credited to the English physician William Harvey, it was al-Nafis who first mounted the challenge to the received wisdom of ancient Greece. So, who was he? And why does he hold a special place in some doctors’ hearts?
Audio brought to you by curio.io
Before we get to know him better, we need to take a side-trip back to 1628, when a 50-year old Harvey published a short but revolutionary treatise. In 80 succinct pages, Harvey succeeded in correcting the reigning and almost sacrosanct theory of blood circulation in his time, put forward by the 2nd century CE Greek doctor Galen, who commanded utmost authority in medicine. Galen’s unparalleled success as a doctor to the gladiators of Pergamon—and his appointment as physician to the emperor Marcus Aurelius—gave him a prestige that no other doctor achieved in the ancient world. His excellent service to the throne led Aurelius to celebrate him as “first among doctors.” The rank and honor stuck as dogma for a millennium.
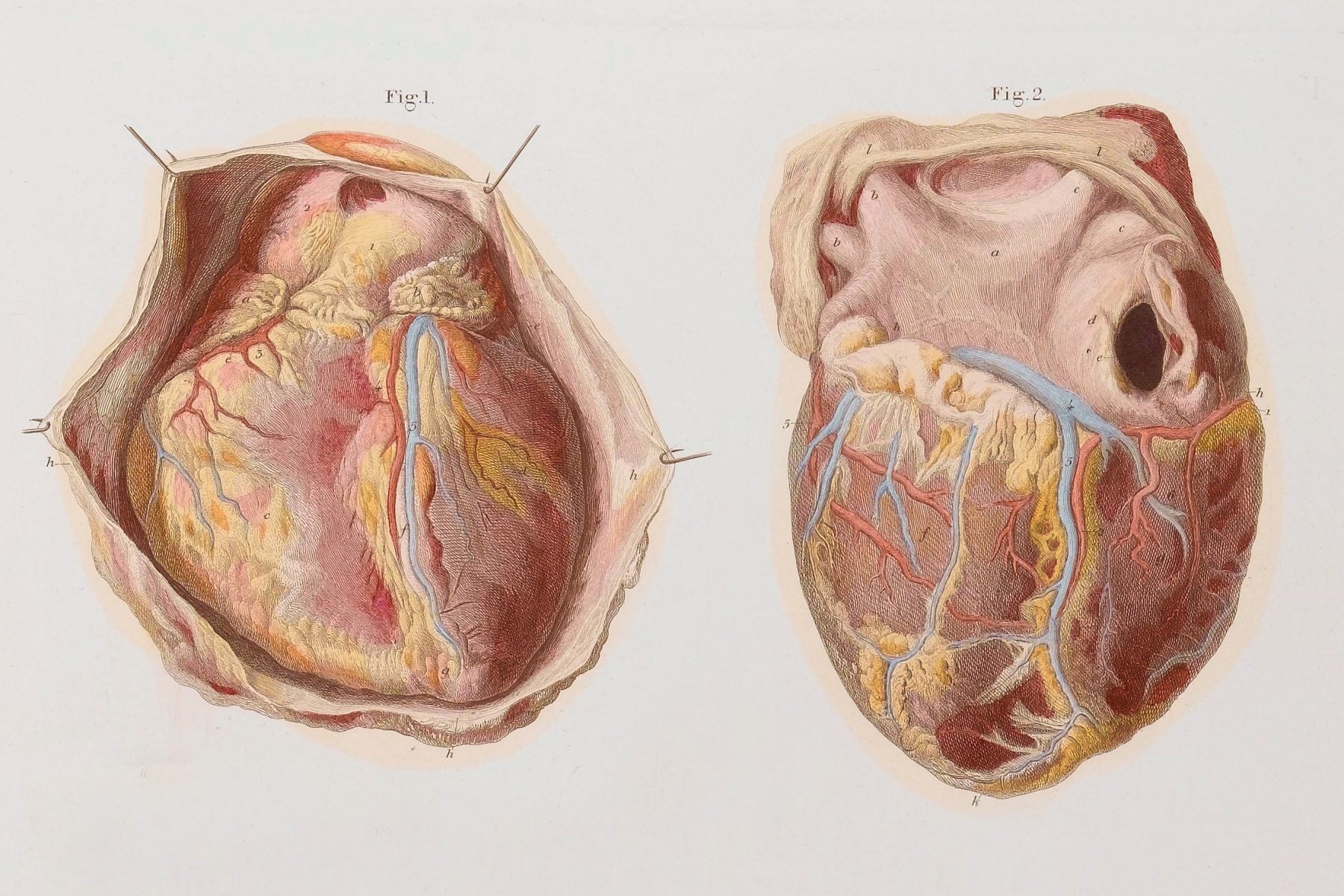
Galen’s Anatomy
In Galen’s system, there was a middle membrane called the septum between the heart’s two ventricles. Galen believed that the septum had invisible pores that permitted the movement of blood from the right ventricle to the left. This perforated passage was an essential feature in Galenic anatomy, which held that blood movement was centrifugal and not circulatory. Blood rushed through the vessels in a one-way trip away from their central origins. Blood transported to the kneecaps, for example, was absorbed by the tissues around the patella, never to be seen again. If blood was constantly consumed, then it was also necessary that the body produce it perpetually. Galen assigned one organ to do just that: the liver.
In her biography of Galen, The Prince of Medicine, the historian Susan Mattern explains that for Galen, “[t]he liver was the central organ of nutrition.” The liver processed and converted food sent from the stomach into nutritious dark blood. Once this type of blood was produced, it was immediately distributed to the body through channels called veins. As Mattern explains it: “In Galen’s system, the liver was the source of the veins.” In other words, veins branched out from the liver, which delivers blood. The pumping effect of the heart was therefore unnecessary, as the blood exiting the liver travelled independently by ebbs and flows through the veins.
In Galen’s anatomical design, the heart’s right ventricle receives a steady supply of blood via a venous channel from the liver. Part of the blood goes into the lungs where it is cleaned, and unclean substances are then exhaled. The rest of the blood passes through the supposed pores into the left ventricle, where it awaits further instruction. Recently purified blood then gets sent out from the lungs into the left ventricle, mixing with the blood that moved over earlier. Now blended, they are then pushed out via the arteries.
Harvey’s Challenge
For Harvey to dispel Galen’s system, he first needed to disprove the existence of a porous septum, as this was the mechanism that allowed Galen to bypass the need for circular blood movement. Luckily for Harvey, someone else had already started the process of critiquing Galen’s system.
A sixteenth century exposé by the Flemish anatomist Andreas Vesalius revealed that Galen based many of his anatomical findings on animal dissections. In Galen’s time, opportunities to study human cadavers were hampered by local beliefs and taboos, so animal analogues were the next best thing. Physicians found this problematic, since the primary subjects of medicine were and are humans. This set the stage for a later series of reviews and criticisms of the Galenic corpus. In his defense, as the classicist and historian of medicine Vivian Nutton notes in Ancient Medicine: “Galen was conscious of the problem of extrapolating from animals to human beings, often warning his audience about drawing rash conclusions solely from animal dissections.”
Correcting Galen’s mistakes required lots of human dissections. Vesalius tore open curtains of skin and welcomed the world to the intramural spectacle of the human body in what is now considered a medical classic, De humani corporis fabrica libri septem (On the Fabric of the Human Body in Seven Books). Published in 1543, this tome empirically presented and detailed the many anatomical errors in Galen’s system. One specific target was Galen’s porous middle: “I do not see how even the smallest amount of blood could pass from the right ventricle to the left through the septum.”
Harvey’s dissection of Galen’s anatomy was two-pronged: observational and experimental. As physician to King James I, and a reputed doctor in the academy, Harvey had access to many animal samples and human cadavers. With the proper intellectual approach, a more liberal view of dissections, and material and financial support, Harvey thoroughly compiled his arguments, producing his 1628 text, Exercitatio anatomica de motu cordis et sanguinis in animalibus (Anatomical Studies on the Motion of the Heart and Blood).
Harvey’s tone is strong and stern. He doesn’t hide his frustrations with Galen. Regarding the supposed permeable septum, Harvey echoes Vesalius in a more forceful voice. After many fruitless searches, he declares: “But, damn it, no such pores exist, nor can they be demonstrated!”
Not only was the physical existence of the septum problematic to Harvey, he was also vexed by its physiological implications:
Even so, supposing the pores are there, how could the left ventricle draw blood from the right when both ventricles contract and dilate at the same time? …Why require invisible pores and obscure uncertain channels to get the blood to the left ventricle when there is such a wide open passage through the pulmonary vein? It is certainly remarkable that a way had to be made, or rather invented, through the dense, tough, and compact septum of the heart, instead of through the open pulmonary vein, and the soft spongy mass of the lungs.
Having closed the imaginary septum and its pores, Harvey proposes a circular route from the right ventricle to the left. This he first surmised after deliberating the blood production role Galen gave to the liver:
For a long time I turned over in my mind such questions as, how much blood is transmitted, and how short a time does its passage take. Not deeming it possible for the digested food mass to furnish such an abundance of blood, without totally draining the veins or rupturing the arteries, unless it somehow got back to the veins from the arteries and returned to the right ventricle of the heart, I began to think there was a sort of motion as in a circle.
To support his supposition, Harvey conducted a series of experiments that involved dissecting various animals, ligating their arteries and veins, exerting pressure on their hearts, and quantitatively measuring the amount of blood channelled to and fro. After having gone through the motions and reviewing his data, Harvey came to a conclusion that debunked both Galen’s passable septum and his blood-producing liver:
It has been shown by reason and experiment that blood by the beat of the ventricles flows through the lungs and heart and is pumped to the whole body… This occurs in such an amount with such an outflow through the arteries, and such a reflux through the veins, that it cannot be supplied by the food consumed. It is also much more than is needed for nutrition. It must therefore be concluded that the blood in the animal body moves around in a circle continuously, and that the action or function of the heart is to accomplish this by pumping.
Harvey’s work was highly revolutionary. Despite being hounded by his contemporaries for contradicting Galen, Harvey helped advance medicine by promoting experimental and empirical methods, free from established dogma. His work also had the effect of introducing mathematics into medical and anatomical research.
Ibn al-Nafis’ Earlier Discovery

But pop history has elevated Harvey’s stature to the level of myth, a hero that was first in many things, especially in raising the voice of reason against Galen. The claim can be easily disputed by mentioning Vesalius’ earlier work. But Vesalius’ corrective was more general, and in the realm of the heart and blood, it was neither Harvey nor Vesalius who first contested Galen: The first rebellious voice to settle the heart of the matter was Ibn al-Nafis.
Born Ala al-Din Abu al-Hassan Ali Ibn Abi-Hazm al-Qarshi al-Dimashqi in 1213, al-Nafis was a man of many minds. He wrote about astronomy, legal theory, philosophy, sociology, and medicine, a subject on which he wrote commentaries and criticisms prodigiously.
Published in 1242, when al-Nafis was only 29 years old, his Commentary on Anatomy in Avicenna’s Canon contains his contentions. In this text, al-Nafis did not just predate later anatomists in resisting Galenic influence, he also made independent discoveries. He was the first to describe pulmonary circulation in print, explaining how blood from the right ventricle enters and exits the lungs. He also discovered the coronary arteries and, in doing so, the mechanisms of coronary circulation, the process by which the heart pumps blood onto itself via coronary arteries that wrap around it.
He first set out to argue, like Harvey, that a porous middle membrane didn’t exist. From his dissections of animals, al-Nafis found that the inner linings of what Galen thought of as the septum were too thick to permit gas exchange (JSTOR). Al-Nafis writes:
…there is no passage as that part of the heart is closed and has no apparent openings as some believed and no non-apparent opening fit for the passage of this blood as Galen believed.
He adds, almost as a flourish, a strong conviction against those who shared Galen’s idea of the septum:
The contention of some persons to say that this place is porous, is erroneous; it is based on the preconceived idea that the blood from the right ventricle had to pass through this porosity–and they are wrong!
Despite his strong contentions against Galen, al-Nafis’ work fell silently into historical obscurity, and his name was shrouded in anonymity for centuries. We can only speculate as to why. But his voice was heard once again, not in a hospital, university, or in a surgery room. In 1924, the young Egyptian physician Muhyo Al-deen el Tatawi was scouring the shelves of what is now the Berlin State Library for his doctoral dissertation. Among the books that he chanced upon was Ibn al-Nafis’ Commentary. This fortunate find restored Ibn al-Nafis to his rightful place in the history of medicine.
Since pop history prefers to embellish its tales with the dramatic, who was first is often a juicy angle in its chronicles. But while Ibn al-Nafis rightly deserves the distinction for being the first to discover the workings of the heart, falling into the trap of pitting him against Harvey is unnecessary. Both deserve recognition for their works. But there is a unique lesson latent in Ibn al-Nafis’ eventual rediscovery, and we should (if you’ll excuse the pun) take it to heart: There are things we think only we know that actually were already known for a long time.