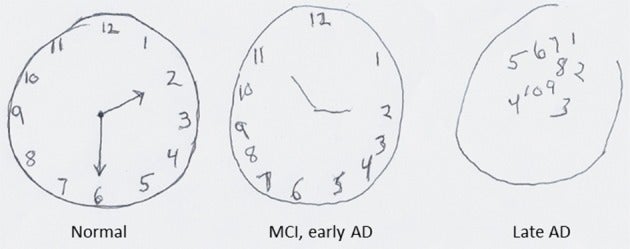
Draw a clock. Start with a round face. Make sure it’s large enough for all the numbers. Then, add hands, setting the time to ten after eleven.
Those are typical instructions for a clock drawing test, a widely-used clinical technique for evaluating cognitive impairment and screening for dementia. The task can be done with just pen and paper in minutes, and usually patients don’t mind being asked to take it up.
“As a cognitive screening test generally, especially for dementia, it has a lot of advantages,” says Kenneth Shulman, a professor of psychiatry at the University of Toronto’s Sunnybrook Health Sciences Centre, who helped develop and popularize clock drawing for that purpose. “It’s easy, it’s cheap—but you have to know how to interpret it. You have to be careful.”
Alzheimer’s disease and other forms of dementia affect at least five million people in the United States, and easily ten times as many worldwide. Most of them are older; past the age of 65, the risk of developing dementia increases over time. Screenings must balance the potential benefits of early detection with the downsides of misdiagnosis, overdiagnosis, and stigmatization.
Weekly Newsletter
The test seems simple, and in many ways, it is. That’s part of its appeal to clinicians. But there is no medical consensus on the details of the clock drawing test—how it’s administered, how it’s scored, who should take it, and who has access to results.
Clock drawing has also entered the public imagination somehow, becoming shorthand for testing cognitive decline. In 2018, when then-president Trump boasted of cognitive test results, many stories fixated on clock drawing as much as any other element of the examination. Shulman is among many clinicians who express curiosity at the specific focus on clock drawing, one of many elements used in clinical cognitive evaluations. As both a medical tool and a bit of folk psychology, clock drawing can reflect concepts of normal aging versus cognitive impairment, as well as difficult-to-encapsulate ideas of personhood, or how a society chooses to care for the elderly.
Experts who use the test daily—even extol its virtues—emphasize the importance of recognizing its limitations. As part of a longer evaluation, Cynthia Munro, a neuropsychologist at the Johns Hopkins Memory and Alzheimer’s Treatment Center, asks most of her patients to draw a clock, which is scored on a Shulman five-point scale. “I sometimes wonder if its popularity exceeds how good it really is, because it’s one item,” she said.
A Brief History of Drawing Clocks
Researchers have traced the origins of clocks in cognitive assessments back to 1915, and the British neurologist Henry Head. In the middle of the first World War, Head became interested in traumatic brain injuries and aphasia, any difficulty in understanding or producing language, and among other basic tasks, he asked patients to read and set clocks. He later said this was “a splendid method of revealing [a patient’s] disabilities.” Head noted that with some patients, “the hands of a clock may be set to an order given in figures, but not when it is expressed in words.”
In 1953, the British neurologist Macdonald Critchley published an influential book on the parietal lobes, a major brain region associated with multiple functions including spatial awareness, touch, and language, that gathered decades of behavioral research. He described what may be the first example of a freely drawn clock test, which has become the dominant form.
Two decades later, in the 1970s, Edith Kaplan, a neuropsychologist at the Boston VA Medical Center, incorporated clocks into widely-adopted diagnostic tests. Clock drawing was a favorite of Kaplan’s, who would administer the task alone if short on time. It was part of what became known as the Boston process approach, a framework for cognitive evaluation that emphasizes how patients arrive at a response more than the answers themselves. For example, Kaplan favored a clock set to 11:10, because it could reveal a common error of literalizing the numbers, pointing the hands to ten and eleven.
Shulman first encountered the clock drawing test in passing while studying geriatric psychiatry in the United Kingdom in the late 1970s. He decided to try it with a patient he suspected had been overmedicated. After an antidepressant was discontinued, Shulman continued to ask the patient to draw clocks, and the series of images showed gradual improvement.
“I said, ‘Hey, this test is sensitive to cognitive change,’” says Shulman. “Clinicians only have to look at the [medical] chart.” He later tested the clock drawing test with a standard cognitive screening instrument and showed that it was useful for dementia screening. In 1986, he co-authored the first systematic study of the test as a cognitive screening for dementia and other cognitive disorders.
One Cognitive Test of Many
Yet there isn’t just one clock drawing test clinicians use, which makes generalizations difficult. Since Kaplan and Shulman adopted and popularized this test, researchers have developed dozens of protocols and scoring systems. Some isolate aspects of the drawing or patient behavior, rated on a multi-point scale. Some provide a circle to be filled in. Some protocols don’t suggest a specific time to use. Some also ask the patient to copy a clock.
Often, a clock drawing is used in concert with alternative screenings such as the Mini Mental State Examination (MMSE) or the Cognitive Abilities Screening Instrument (CASI), or incorporated into a larger battery of questions and tasks, such as the Montreal Cognitive Assessment or Mini-Cog screening.
Shulman has recently embraced a simpler-is-better philosophy, encouraging a screening version of the test that relies on basic intuitive judgments. “Is it normal, abnormal, or different than what was done [by the patient previously]?” he says. “It’s limited, but it’s a very useful test.”
New variants of the clock drawing assessment are still being developed. For example, computerized tests conducted on tablets can collect additional data, such as reaction time or stylus motion, then analyze drawings and data with artificial intelligence.
“I hope that our ability to detect these cognitive biomarkers is going to contribute to preventing a lot of cost and suffering and disease,” says Rod Swenson, a neuropsychologist based in Fargo, North Dakota, who has consulted with Linus Health, a digital health company, on the development of an iPad version of the clock drawing test.
Elena Tsoy, a neuropsychologist at the University of California, San Francisco, who has developed computerized versions of other cognitive tests, says that access to remote healthcare is sometimes inequitable, but when computer tests are deployed in clinic settings, they offer the ability to reliably measure cognition without requiring providers’ time; can be highly standardized; and ultimately should expand access to specialist care.
Time Limits
Cognitive tests are rare in non-specialist situations, says Munro, but any cognitive assessment is not necessarily better than none, with special concern for false negatives and false positives.
In theory, annual clock drawings could establish a baseline of performance for a patient, but the task alone might not provide enough evidence for useful conclusions. “I’m not convinced that clock drawing is a sensitive enough measure to detect early change,” says Tsoy. Some studies have found that clock drawing does not reliably pick up on mild cognitive impairment.
Munro sees the same pattern in her patients, who are typically at the mild end of the spectrum of cognitive impairment. “Usually people can do it well. If they can’t do it, that tells me there’s more going on,” she says. “More” could be a sign of dementia, but it could also be something else, such as vision or motor problems. Experts caution against non-specialists leaping to conclusions over what appears to be a poorly drawn clock.
And clock drawing may not work equally well for everyone. Education level has repeatedly surfaced as a factor in performance, and education differences may be tied to clock drawing differences in multicultural populations. “When it comes to people we evaluate who come from different backgrounds, we have to be more careful,” says Tsoy, “We should not presume that these tests mean the same things to them as to the population in which these tests are developed.”
For example, a relationship to time that relies on clocks could easily be taken for granted, but they might be less important to a farmer, or someone from a place where clocks are used less frequently. Investigators have tried to develop evaluations which test similar cognitive skills that work in settings where clock drawing has struggled, such as the papadum test, which asks patients to fold a paper disc into six equal parts.
Cultural differences also span time. Evaluations must account for normal aging and cognitive decline. Shulman is often asked about clock drawing losing efficacy over the coming decades now that the ubiquity of analog clocks and watches has waned. “It’s still a useful test for the rest of my life,” he says. “What happens after I’m gone is not my problem.”
Advice on regular testing of any sort is mixed. The American Academy of Neurology, among other organizations, recommends annual screenings for cognitive decline for all adults over the age of 65. The U.S. Preventive Services Task Force considers the evidence insufficient to either recommend or discourage screening asymptomatic adults. Patients and their own families are sometimes at odds over dementia diagnosis disclosure.
Other concerns about clock drawing apply broadly to all cognitive assessments, including what might be called pre-diagnosis and poor incentives. Sources for this story favored earlier detection, with parallel efforts to improve other aspects of care and access.
“Most of my career was spent giving people bad news: ‘What you have sucks and it’s going to get worse,’” says Swenson. “I’d like to change that.”