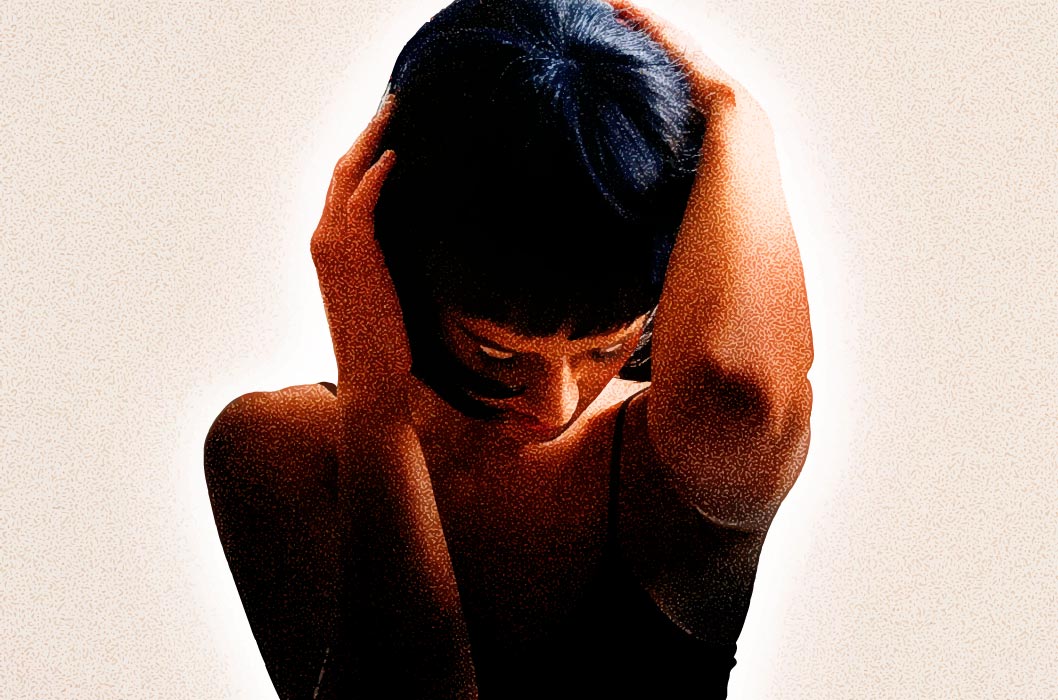
In light of the high rates of suicide and general mental-health struggles among teens, the American Academy of Pediatrics has recommended that everyone ages 11 to 21 be annually screened for depression. They’re also actively working to develop guidelines for how this should be handled.
Kids and young adults aren’t the only ones under scrutiny: a government-appointed health panel has suggested that women be screened for depression during pregnancy and after giving birth. According to The New York Times, this panel gave the recommendation a “B” rating, which means that such a screening must be covered under the Affordable Care Act.
Though mental-health and depression are serious issues, implementing routine depression screenings can be complicated. Researchers Simon Gilbody, Trevor Sheldon, and Simon Wessely, writing in the British Medical Journal, argue that depression screenings can be fairly inaccurate, expensive to administer, and can lead to many false positives.
The researchers acknowledge that depression is a serious problem that affects anywhere from 8% to 12% of the general population, and that many people with depression go undiagnosed. However, one possible downside to routine screenings, the researchers suggest, is that they do not always take severity into account. Results can also be dependent on the timing of tests. For example, in some cases, screenings have identified people as depressed, but upon follow-up, a good number of the same patients had resolved their issues within two to four weeks. Thus, for mild to moderate depression, they argue, it’s important to watch a patient over a period of time before implementing treatment.
Even if the rates of accurate diagnoses increase, it is unclear whether the patient’s outcomes will improve. In general, patients with undetected depression tend to have milder forms of the illness, and these milder forms sometimes can be resolved individually without significant intervention. Typical interventions for depression include therapy and prescription anti-depressants, which may not only be useless for mild cases, but, especially with regards to anti-depressants, possibly dangerous. Thus, the costs of routine screenings and the time and effort to bring patients in may not ultimately prove useful relative to the benefits of treatment.