The idea that death should be merciful is not new. When a person is gravely wounded or terminally ill, when death is inevitable, and the suffering is so great that living no longer brings any joy to the person, it is understandable that he or she may wish to die. In “Two Pioneers of Euthanasia Around 1800,” Michael Stolberg cites accounts of people pulling on the legs of those who had been hanged, but had not yet died, to hasten their deaths. He mentions also Apologie, the autobiography of a French surgeon named Ambroise Paré who happened upon three gravely wounded soldiers. An uninjured soldier asked the surgeon if they would live, to which he responded they would not. The uninjured soldier proceeded to slit their throats.
The invention and widespread use of morphine in the 19th century to treat, and then to kill, pain led to the belief that a less painful dying process was possible, Giza Lopes writes in her book Dying With Dignity: A Legal Approach to Assisted Death. In the mid-19th century, surgeons began using chloroform, which had fewer negative side effects than morphine, and which knocked people unconscious. In 1885, the American Medical Association officially opposed voluntary euthanasia. Though some doctors believed in the redemptive nature of suffering, the opposition was not overwhelming enough to stop the movement. The ability to relieve pain experienced as the result of surgical procedures, childbirth, or mere living, logically led to conversations about death and dying. Medications could alleviate end-of-life suffering and expedite death.
As time and technology progressed, everyday people came to see physicians as godlike figures, and, Lopes writes, doctors claimed a role in the process of dying. Through the early 20th century, opiates were still widely available, but physicians had begun to take control of prescribing and administering other medications.
On January 23, 1906, the Ohio legislature introduced a euthanasia bill. A Cincinnati woman named Anna Hall had lobbied hard to legalize euthanasia, hoping to hasten the death of her mother, who was suffering from a terminal and painful illness. That same year, Dr. R. H. Gregory introduced a similar bill to the Iowa state legislature. These two have been dubbed the “chloroform bills.”
Doctors and ethicists from both the United States and England hashed out their thoughts on euthanasia in medical journals, and the movements in both countries evolved in tandem. When Dr. Gregory proposed the Iowa euthanasia bill, the British Medical Journal responded, tearing into him:
That the man is either a crank of a particularly noxious type or a mere-notoriety hunter, is clear enough from the statement attributed to him that he simply wishes to make lawful that which is already daily practised by the greatest physicians and surgeons in every large hospital in the United States. If Dr. Gregory really believes this, he is more credulous than the simplest gobe-mouche who swallows without straining the ‘platform facts’ of antivivisection and antivaccination; if he does not believe it, he is a liar of the basest kind.
A few years later, in 1911, a woman named Sadie Marchant, who was living in a Shaker colony and struggling to breathe with a single functioning lung for years, asked for help dying. The Shakers with whom she’d been living prayed and decided finally that helping her die would be the right thing to do. Two of the Shakers were arrested. Their case was ultimately dismissed in January 1912, Lopes writes in Dying With Dignity. The case was well covered by newspapers across the country including the Washington Times and the New York Times. The dismissal of charges helped cement the idea of “euthanasia” as merciful in the case of terminal illness and grave suffering.
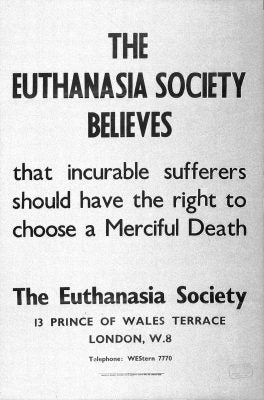
In 1935, the euthanasia movement got going in earnest in England when the Voluntary Euthanasia Legalization Society was founded. It held its inaugural meeting that year, and the society’s founder, C. Killick Millard, wrote to the British Medical Journal that he hoped the British Medical Association, which had not offered an opinion one way or another, would not offer an opinion. The decision to die, the author continued, was not a medical one.
A bill was introduced to Britain’s House of Lords in 1936 that would allow anyone over 21 years old who was mentally competent and fatally ill, or sick with an incurable disease, and suffering from immense pain to request voluntary euthanasia. The person would have to have two witnesses and be seen by several doctors, and then apply to the Minister of Health, who would then have to interview the dying person. That bill’s requirements are nearly identical to the ones that are now law today in several U.S. states. With 35 to 14 votes, the bill was defeated.
In 1957, the Vatican proclaimed that passive euthanasia was acceptable, according to Thomas R. Cole’s review of A Merciful End. Passive euthanasia is the deliberate decision to withhold lifesaving measures, like a ventilator, knowing that death will result. Hoping to take advantage of the change in public opinion after the Pope’s declaration, assisted-suicide advocates pivoted to focus on legalizing passive euthanasia.
Fast-forward four decades to 1994, when Oregon became the first state to legalize aid in dying. The law was immediately challenged, Lee v. State of Oregon. The case made its way through the court system for the next three years, and in February 1997, the Ninth Circuit Court of Appeals dismissed the lower court’s ruling against the Oregon Death with Dignity Act. The law went into effect in 1997.
Around the same time, Dr. Jack Kevorkian was traveling across the country with his “death machine,” making the cover of Time and stirring up conversation about end-of-life choices. District attorneys brought criminal charges against Kevorkian for ending people’s lives several times, but he was convicted only once. Kevorkian had filmed himself giving a man with amyotrophic lateral sclerosis (ALS) life-ending medication. He then gave the tape to Mike Wallace, host of 60 Minutes. Wallace aired the tape on TV alongside an interview with Kevorkian. In the tape, after the man dies, Kevorkian challenges the district attorney to take him to court. Reluctantly, the DA did, and this time Dr. Death lost. Kevorkian was sentenced to between 10 and 25 years in prison, the New York Times reported in his obituary. He was released in June 2007, after promising he’d never help in another suicide. He died in 2011.
* * *
Today, anyone choosing to die under the law in states where physician aid is legal, like Oregon, Washington, Vermont, Montana, and California, must be able to self-administer the life-ending medication. If the patient cannot, then he or she is ineligible, which means that most people suffering from neuromuscular diseases like ALS and Parkinson’s will not be able to ease their pain legally. By the time people with these diseases are within six months of death, more often than not, they cannot self-administer.
That said, some doctors are still willing to help patients die, whether legally or illegally. In non-Catholic hospices, as in those associated with the Church, palliative sedation—like the so-called passive euthanasia of yore—is one way doctors help their patients hasten death. The “doctrine of double effect” safeguards doctors whose good-faith actions result in the death of their patients. If the doctor can make the case that he or she administered medicine without knowing or not believing it would result in a patient’s death, the doctrine protects them.
As medical technology gets better and better, death can become more prolonged and more difficult. A heart attack that once might have killed a person can now serve as a “wakeup call.” Ventilators keep people breathing far beyond when their bodies would have died naturally. Death does not come as it used to. While some people might welcome more days, regardless of their pain or diminished physical state, others do not. Policy and medical ethics have not kept up with technology.
Editor’s Note: The penultimate paragraph of this story was edited to clarify that Catholic hospices have Vatican approval to use palliative sedation.