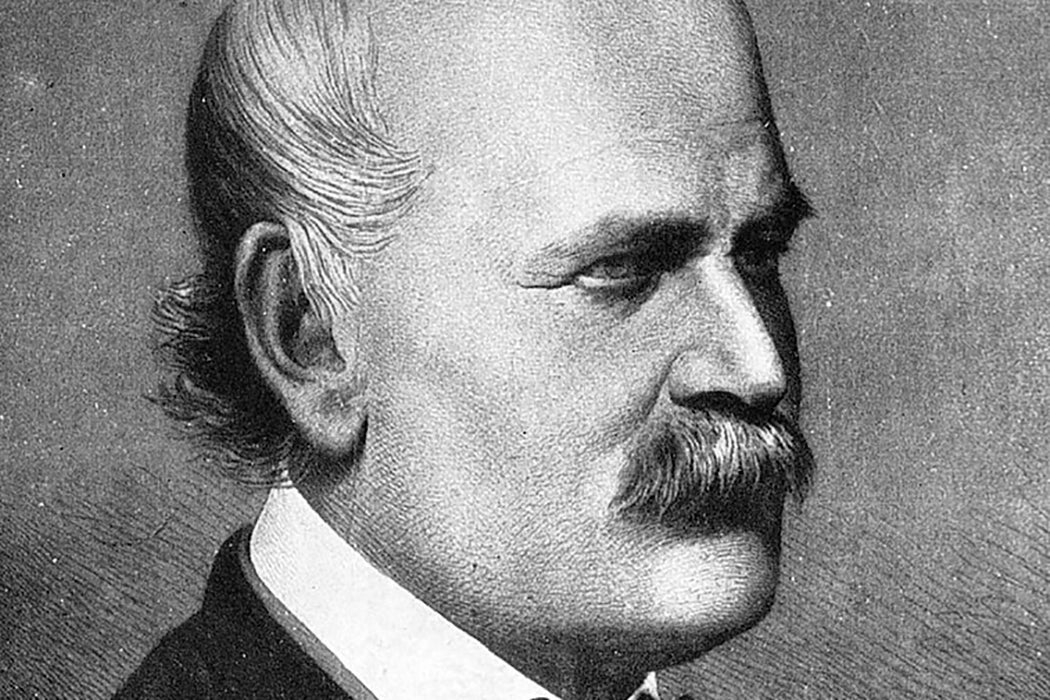
Ignaz Semmelweis is known as the nineteenth-century doctor who discovered the cause of childbed fever, the devastating illness that often struck women shortly after childbirth and killed scores of mothers and babies. His solution was that doctors should wash their hands. Sounds simple, but it was revolutionary at the time, and has formed the foundation of modern infection control.
The story that persists about Semmelweis is that he was a tragic hero felled by a medical establishment that refused to recognize a ground-breaking discovery capable of saving thousands of lives. In this iteration, he was a man on a noble mission to spread the word of his simple intervention that spared mothers and babies from a fearsome death, only to be laughed at by his colleagues like some latter-day Don Quixote. Semmelweis’s obsession with proving his theory allegedly drove him to madness, and then death.
But that’s not quite true.
A New Era of Medicine
Vienna in the middle of the nineteenth century was a city undergoing a revolution, and that revolutionary spirit found its way into the halls of the Vienna Medical School. The medical field was at a turning point. The famed surgeon Theodor Billroth described the older generation of doctors as “a generation that has been reared in an intellectual strait-jacket with dark spectacles before their eyes and cotton wool in their ears.” In the struggle between young and old, Semmelweis was a member of this vanguard ushering in a new era of medicine that used clinically-derived evidence to treat patients. Radiologist T. Doby writes that these new tools of science—observation, the collection of data, logical analysis—helped Semmelweis to understand childbed fever, also known as puerperal fever.
Weekly Newsletter
All retellings of the doctor’s breakthrough begin the same way. The Vienna General Hospital had two maternity wards. Semmelweis observed that childbed fever afflicted more women in the first division, which was staffed by (male) doctors and medical students, than in the second division, where midwives attended the women. According to scholar Douglas Allchin, over the course of several years, Semmelweis conducted an observational study of the two maternal wards, meticulously isolating one variable at a time. He then performed a logical analysis of his compiled data to determine the cause of puerperal fever. The source of the infection was the doctors themselves. They would perform autopsies, often on women who had succumbed to the fever, and then, without washing their hands, would perform exams on laboring women, passing the illness from mother to mother.
Here’s where the stories diverge. The popular narrative, still commonly repeated in mainstream retellings of the story, says Semmelweis faced a universal backlash against his ideas. But in fact, his methods were in good company. Semmelweis was using what he learned at the medical school where he was now an assistant professor. His mentor, Karl von Rokitansky, had introduced the study of pathology into the university’s curriculum. There was a direct line from the 30,000 autopsies Rokitansky performed to develop his understanding of human pathology to Semmelweis’ intensive observations and data gathering.
Semmelweis’s Missteps
So, if Semmelweis was not simply a genius ahead of his time who was ignored by the academy, why didn’t his ideas catch on?
Semmelweis scholars almost always point to the extended length of time it took him to author his full findings as one reason his theories didn’t gain traction. Then, as now, academic careers rose and fell based on one’s ability to publish one’s work, and by failing to do so, Semmelweis kept his ideas from finding a large audience.
Why he didn’t publicize his findings once his handwashing protocol was implemented is unknown, but we do know that the first mention in print came from a close friend and fellow practitioner of evidence-based medicine, Ferdinand von Hebra. The majority of the leadership of the Vienna Medical School supported Semmelweis’s work; the recognition from his prestigious peers gained him admittance to Austria’s Academy of Sciences. Bioethicist Sherwin B. Nuland notes that when Semmelweis finally spoke about his discovery to the Medical Society of Vienna in 1850, his presentation was considered a resounding success. Semmelweis’s ideas about the transmission of puerperal fever were being debated and discussed in Europe’s centers of medical knowledge. It was the best-case scenario that all researchers hope for.
But again, he failed to publish.
Want more stories like this one?
Semmelweis had a significant obstacle that kept him from effectively translating his ideas: he didn’t speak the language very well. He had grown up speaking a regional dialect in his native Hungary and didn’t learn proper Hungarian until secondary school. When young Semmelweis arrived in Vienna to study medicine, he again had to pick up a new language, but never wholly mastered the German of his Viennese colleagues.
Additionally, in the pecking order of medical specialties, obstetrics fell low on the totem pole. Pregnancy and childbirth were still considered to be the purview of women, and so didn’t attract much attention or acclaim in the schools or salons where medical advancements were debated and disseminated.
A Precipitous Decline
These are valid obstacles, but modern scholars, re-examining the work of Semmelweis with the benefit of time and distance, have generally concluded that the bulk of the blame for Semmelweis’ failures lands squarely on his shoulders. According to philosopher Dana Tulodziecki, by leaving it to his colleagues like Hebra and Rokitanskey to publicize his discoveries, he relinquished control over the interpretation of his work. His surrogates often missed subtle but essential aspects of the work, like the fact that Semmelweis had not just shown that puerperal fever was contagious (which was already a widely-accepted fact), but had identified the mode in which it was transmitted from the unsanitized hands of doctors to laboring women. Even more extraordinary was that Semmelweis deduced that puerperal fever was not an illness exclusive to postnatal women, but an expression of the same infection that caused blood poisoning in post-operative patients or the feverish death of a laborer who had initially presented with a non-life-threatening open wound.
When he did finally publish his magnum opus, The Etiology, Concept, and Prophylaxis of Childbed Fever, in 1860, his chance to make an impact with his work had passed. He was no longer at the center of the medical world in Vienna but had taken a position at the much-smaller University of Pest, in his native Hungary. Always mercurial, Semmelweis became paranoid and unstable. He wrote angry, rambling letters to those who dismissed or disagreed with his theories, calling them “murders” and “butchers” of women.
Narratives that celebrate the Semmelweis mythology cite this irrational behavior as proof that the doctor’s obsession with saving women from the specter of childbed fever had driven him mad. But evidence shows that he was more likely suffering from early-onset Alzheimer’s. This, not some descent into insanity, was probably why his family had the 47-year-old doctor committed to an asylum in the summer of 1865, where he died a few short weeks later.
It seems likely that Ignaz Semmelweis died from the effects of a beating inflicted by asylum guards trying to restrain him. Some accounts of his death, however, report that he died of septicemia, the same condition his work had attempted to prevent.